 Non-alcoholic Fatty Liver Disease
Non-alcoholic Fatty Liver Disease
What is NAFLD?
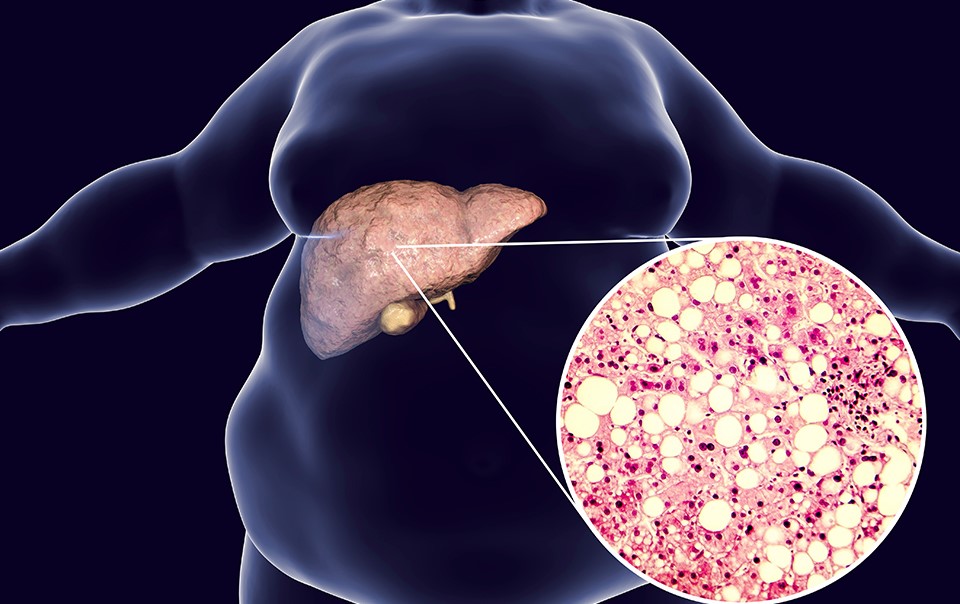
NAFLD stands for non-alcoholic fatty liver disease. It is an umbrella term that covers a range of fatty liver conditions, including NASH (non-alcoholic steatohepatitis). NAFLD is defined by the presence of droplets of fat in the liver cells in absence of alcohol or medication-related causes. Recently, people have started using the term MAFLD (metabolic-dysfunction associated fatty liver disease) in recognition that is can occur in the presence of other liver conditions including alcohol use.
Who gets NAFLD/ why am I affected?
NAFLD is common, affecting more than a quarter of adults in most parts of the world. It is closely associated with:
- being overweight or obese
- type 2 diabetes
- high blood pressure (hypertension)
- dyslipidaemia (abnormal levels of fats in the blood, including cholesterol levels)
- sedentary lifestyle
Is it serious?
In the majority of cases, NAFLD is not serious and the fat in the liver does not cause additional problems. It can be a “wake-up call” for people to improve their health as the same things that cause NAFLD also increase the risk of cardiovascular diseases such as heart attacks and strokes. Importantly, however, there is a substantial minority of people with NAFLD (between 5% and 7%) who develop liver-related complications including advanced fibrosis and cirrhosis, which can lead to liver failure and liver cancer.
How is it diagnosed?
NAFLD does not usually cause symptoms and, if it does, they are non-specific, such as tiredness or dull ache in the upper abdomen. NAFLD is frequently picked up incidentally on tests, such as liver blood tests (“liver function tests”) or an ultrasound scan, requested for other reasons. Doctors and other health practitioners are increasingly aware of the condition, so may look for it in patients with risk factors, such as type 2 diabetes and/or obesity.
When making a diagnosis, the clinician will ask about:
- history of abnormal liver tests or of liver conditions
- alcohol consumption
- any other medications or supplements
- diabetes, blood pressure, cholesterol and any angina, heart attacks or strokes, including in close family members
Investigations include:
- blood tests to exclude other causes of liver disease (including viral, autoimmune and metabolic causes)
- Imaging such as an ultrasound scan
- Tests to assess severity, often including FibroScan®
How is NAFLD treated?
Lifestyle management is the mainstay of treatment including diet and exercise, but the approach is individualised as one size does not fit all. Examples include:
- Calorie counting and calorie restriction
- Reduction in portion sizes
- Reduced snacking, sugary drinks and confectionary
- Reduction in processed foods and refined carbohydrates
- Increase in water, vegetables, fruits and lean protein
Stopping smoking and minimising alcohol intake are also important. Specific diets may be considered according to individual circumstances. Exercise is also very important, but the ability of people to engage in exercise varies. The starting point is increasing daily activity levels, perhaps using a step counting app or wearable technology, moving on to aerobic and resistance training as appropriate.
The next step is to use medications to minimise cardiovascular risk, including attention to:
- Diabetes: using newer therapies that promote weight loss, reduce risk of dying from cardiovascular disease and don’t carry risk of low blood sugar “hypos”
- Blood pressure: keeping blood pressure well controlled using agents with beneficial cardiovascular risk
- Cholesterol: statins tend to be helpful for chronic liver diseases, despite popular belief! They are also helpful in reducing overall mortality
Finally, novel therapies are being developed all the time. The Oxford team conduct a number of clinical trials and some newer drugs may be available to prescribe soon…
